What is Endometriosis

Endo 101: Causes, Symptoms and Diagnosis of Endometriosis
For 176 million people around the world, endometriosis is no joke. It’s the most common gynaecological condition (affecting 1 in 10), and it’s the leading cause of infertility and chronic pelvic pain [1].
Although it’s common, endometriosis is often undiagnosed, misdiagnosed or undiscovered in many menstruators. Symptoms are often dismissed by doctors as “normal” even if they cause distress and impact on the quality of life.
It’s time to take it seriously! Here at ANP, we want you to understand the ins and outs of endo and empower you to be your own health advocate so you can manage your symptoms and live pain-free.
What is endometriosis?
We’ll start with the basics – your endometrium!
Your endometrium is the lining of your uterus, and it’s the fastest growing tissue in your body! It thickens during your menstrual cycle to prepare your body for the implantation of an embryo, and it’s shed during menstruation.
Now let’s define endometriosis.
Endometriosis is a chronic inflammatory disease characterised by the presence of endometrial-like tissue (stroma and glands) found outside the uterus. This tissue grows non-cancerous lesions which can then become scar tissue and adhesions. The lesions are oestrogen-dependent, stem-cell driven, and can be progressive.
Important! → Endometriotic lesions and your endometrium are NOT the same. Endometriotic lesions are different in structure and behavior from your endometrium.
Where are lesions found?
Endometriotic lesions are found mainly on the ovaries, fallopian tubes, bladder, Pouch of Douglas (the small area between uterus and rectum), uterosacral ligaments, and intestines.
Endometriosis can spread anywhere in the body, and in very rare cases, it has been found in the lungs, liver, kidneys, appendix, calf muscles, and even the brain!
What causes endometriosis?
Researchers are not sure of the exact cause of endometriosis.
Genetics seem to play a part as endometriosis may be inherited through the maternal OR paternal line.
Possibly, endo may occur when doctors unintentionally move endometrial tissues during surgeries such as c-sections, hysterectomies, and other abdominal surgeries.
Some research shows an association between endometriosis and people with ovarian or breast cancer [2].
And recent 2020 research found that people with endo have a specific chemical modification to their DNA [3].
Any risk factors?
While the exact cause of endo is uncertain, there is some evidence that environmental factors can potentially contribute to the development or progression of endometriosis.
Factors that may precede the development of endo include:
- Altered gut microbiome [4]
- Pelvic infections
- Stress
- Exposure to toxins [5]
- Alcohol consumption
- Poor diet and lifestyle choices
- Irregular menstrual cycles
- Abnormal structure of cervix, vagina, or uterus
- Autoimmune diseases [6]
- Physical or sexual abuse during childhood or adolescence [7]
Don’t fret! With a few lifestyle changes, you can reduce your chances of developing endometriosis and manage your symptoms.
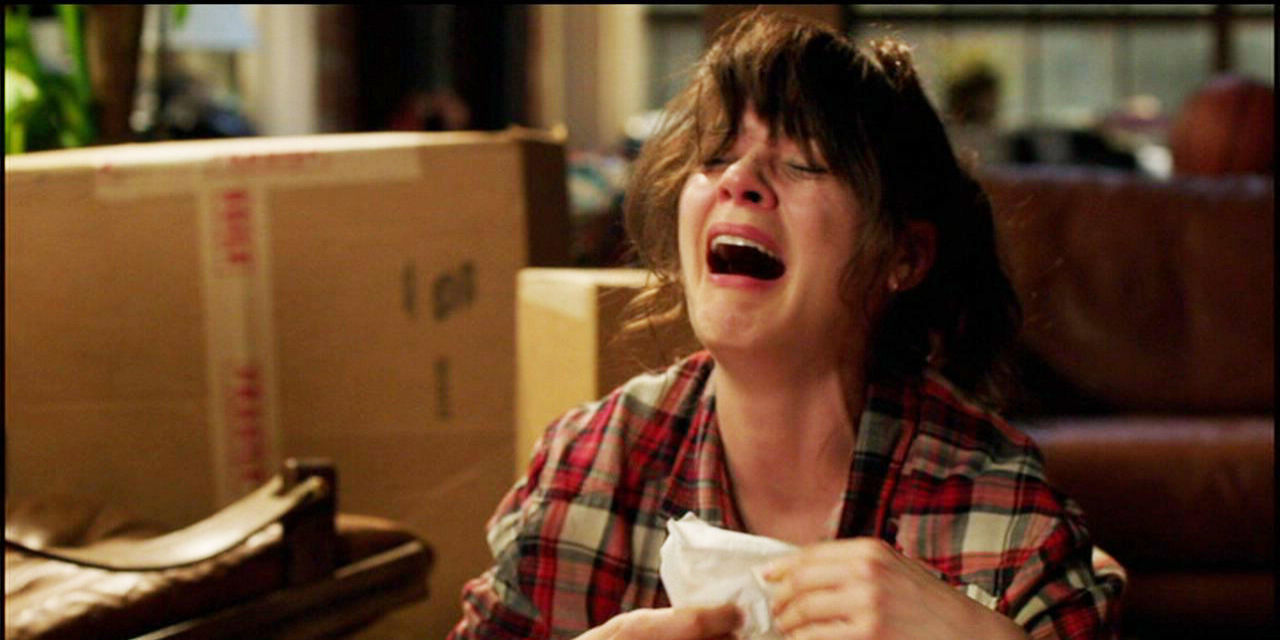
Endo is a pain – literally!
There are various symptoms associated with endometriosis, including:
- Dysmenorrhea (painful periods)
- Mid-cycle pain (during ovulation)
- Bloating (AKA endo belly)
- Infertility
- Rectum pain
- Heavy or clotting periods
- Depression
- Anxiety
- Fatigue
- IBS
- Pelvic pain or back pain
- Shooting pain in legs
- Pain with sex
Infertility and recurring dysmenorrhea are the most common symptoms. The pain from endo can be chronic and excruciating and bring emotional distress during menstruation or sexual intercourse.
Remember! Any pain higher than a 6/10 on a pain scale during your menstrual cycle is NOT normal. Life shouldn’t come to a halt because of debilitating pain. Doctors should take period pain seriously and treat the root cause.
Being diagnosed with endometriosis
A proper diagnosis of endometriosis can be a long process. If you believe you have endometriosis, a specialist will first discuss your symptoms and medical history to determine if you need image testing. They may perform a pelvic ultrasound; however, the only way to know if you have endo is through laparoscopic surgery.
Late diagnosis is common. On average, it takes around 7-10 years for endometriosis to be diagnosed, and the average age for a menstruator to be diagnosed is 28 years old! That’s way too long if you ask us.
Late diagnosis often occurs because many doctors dismiss dysmenorrhea as “normal” and menstruators often don’t know they’re infertile until they struggle to have a baby.
Stages and treatments
Once diagnosed, the severity of endo is ranked in four stages:
Stage 1 – Minimal: a few lesions and little to no scar tissue.
Stage 2 – Mild: several lesions and some scar tissue.
Stage 3 – Moderate: many lesions, possible cysts on one or both ovaries, and adhesions (thick bands of scar tissue).
Stage 4 – Severe: widespread lesions, many thick adhesions, and cysts present on one or both ovaries.
Common treatments include laparoscopic surgery to remove scar tissue and hormonal contraceptives such as Mirena or the Pill. It’s important to remember that while hormonal contraceptives can help lighten heavy periods and reduce pain, they do not stop (or treat) the growth of endometriosis.
Stay strong, endo warriors!
If you have endometriosis or were recently diagnosed with endometriosis, you are not alone! With several endo warriors on our ANP team, we understand all the struggles that come with it. Stay strong! You can live a happy, healthy life with this gynaecological condition. We take your symptoms seriously, and we are here to support you as you manage your endo.
See the science:
- Drseckin.com. Accessed November 6, 2021. https://drseckin.com/infertility/
- Contemporaryobgyn.net. Accessed November 6, 2021. https://www.contemporaryobgyn.net/view/risk-breast-cancer-surgically-verified-endometriosis
- Houshdaran S, Oke AB, Fung JC, Vo KC, Nezhat C, Giudice LC. Steroid hormones regulate genome-wide epigenetic programming and gene transcription in human endometrial cells with marked aberrancies in endometriosis. PLoS Genet. 2020;16(6):e1008601.
- Leonardi M, Hicks C, El-Assaad F, El-Omar E, Condous G. Endometriosis and the microbiome: a systematic review. BJOG. 2020;127(2):239-249.
- M. Freger S, G. Foster W. The link between environmental toxicant exposure and endometriosis re-examined. In: Endometriosis. IntechOpen; 2021.
- Shigesi N, Kvaskoff M, Kirtley S, et al. The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis. Hum Reprod Update. 2019;25(4):486-503.
- Harris HR, Wieser F, Vitonis AF, et al. Early life abuse and risk of endometriosis. Hum Reprod. 2018;33(9):1657-1668.